Abstract
Introduction
Acute myeloid leukemia (AML) is a clonal hematologic malignancy characterized by the proliferation and accumulation of blasts in the bone marrow (BM) which results in hematopoietic failure. Transferrin receptor (CD71) plays an important role by up-taking iron into the cell, and its expression is regulated by cellular iron levels. Recently, CD71 has emerged as a sensitive and specific marker of cell proliferation in solid tumors. The clinical significance of CD71 expression in AML remains unclear. Current efforts are also exploring its potential as a therapeutic target in AML. We aimed to describe the clinical characteristics and outcomes of patients diagnosed with de novo AML who expressed CD71.
Methods
We conducted a retrospective analysis of 453 patients with newly diagnosed AML that came to our institution from December 2019 to June 2021 in whom CD71 antibody was available at diagnosis. CD71 expression was assessed by flow cytometry immunophenotypic studies performed using bone marrow aspirate specimens at presentation. For each analysis, a minimum of 200,000 events was acquired on FACSCanto II instruments (8-color and 10-color, BD Biosciences). The CD45 dim-blast region including monocytes based on CD45 / side scatter was analyzed. The antibody panel included 5 tubes; CD71 antibody was included in tube 3, which contains the following antigen combination: CD41/CD71/CD56/CD34/CD64/HLA-DR/CD14/CD45. The neoplasm was CD71-positive if at least 20% of blasts demonstrated CD71 expression. Additionally, frontline treatment was categorized into intensive chemotherapy (HiDAC based), and Low-Intensity regimen (double nucleoside analog or hypomethylating agent-based therapies). Outcomes in terms of survival and treatment response were analyzed and reported by age, ELN risk groups (Favorable, Intermediate, and Adverse), and the presence of somatic mutations.
Results
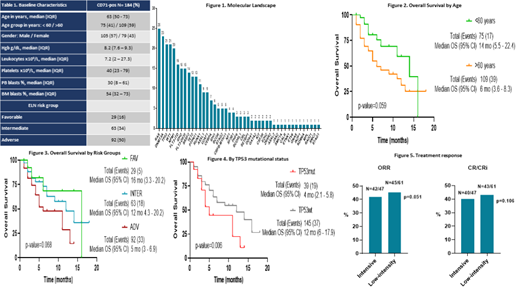
Baseline characteristics are detailed in table 1. We identified 359 (79%) patients diagnosed with AML in whom CD71 was expressed. Our study focused on 184 (41%) patients diagnosed with previously untreated de novo AML, the median age was 63 years (IQR 50-73). Fifty-seven percent of patients were male. Median hemoglobin and platelet counts were 8.2 g/dL and 40 x10 9/L, respectively. The Median BM blast percentage was 54%, among these patients, there was a higher representation of patients with adverse risk features when compared with the intermediate and favorable group (50%, 34%, and 16% respectively). The molecular landscape of our population showed higher representation of RAS (25%), DMNT3A (23%), TP53 (21%), WT1 (21%), NPM1 (20%), FLT3-ITD (16%), and IDH2 (15%), figure 1. Frontline treatment information was available on 108 patients, of these, 43% were treated with intensive chemotherapy, while 57% of patients were treated with a low-intensity regimen.
In terms of outcomes, with a median follow-up time of 6 months, the median overall survival of the whole patient cohort was 9 months (95% CI: 4.3-13.6). Patients aged more than 60 years showed inferior OS compared to younger patients (6 vs. 14 months; p=0.059), respectively, figure 2. Among patients with adverse risk features, the median OS was 5 months (95% CI: 3-6.9, p=0.068) versus those with intermediate (12 months) and favorable risk features (16 months), figure 3. Next, among the somatic mutations with higher representation with known prognostic impact, patients with TP53 mutated showed a significantly inferior OS compared to those with wild type (median 4 vs. 12 months, p=0.006) respectively, figure 4. Patients treated with intensive chemotherapy showed a trend to higher ORR versus low-intensity regimen (89% vs. 74% respectively, p=0.051). Similarly, CR/CRi rates were higher among those treated with intensive chemotherapy compared to those with a low-intensity regimen (85% vs. 70% respectively, p=0.106), figure 5.
Conclusion
Acute myeloid leukemia is an aggressive hematologic malignancy with a heterogeneous nature. CD71 expression appears to be a common event and was identified in up to 40% of de novo AML cases in our institution. Its expression appears to be associated with cytopenias in addition to the presence of molecular abnormalities commonly associated with an adverse prognosis. Its clinical significance, applicability as a diagnostic marker, and potential as a therapeutic target in AML need to be fully elucidated.
Alvarado: Astex Pharmaceuticals: Research Funding; Jazz Pharmaceuticals: Research Funding; BerGenBio: Research Funding; CytomX Therapeutics: Consultancy; MEI Pharma: Research Funding; Daiichi-Sankyo: Research Funding; FibroGen: Research Funding; Sun Pharma: Consultancy, Research Funding. Kantarjian: Immunogen: Research Funding; Astra Zeneca: Honoraria; Ipsen Pharmaceuticals: Honoraria; Jazz: Research Funding; Amgen: Honoraria, Research Funding; Astellas Health: Honoraria; Aptitude Health: Honoraria; Novartis: Honoraria, Research Funding; KAHR Medical Ltd: Honoraria; NOVA Research: Honoraria; BMS: Research Funding; Ascentage: Research Funding; AbbVie: Honoraria, Research Funding; Daiichi-Sankyo: Research Funding; Pfizer: Honoraria, Research Funding; Precision Biosciences: Honoraria; Taiho Pharmaceutical Canada: Honoraria.